Biliary Atresia: Symptoms And Treatment
Biliary atresia is a chronic and progressive liver disease. It becomes apparent shortly after birth.
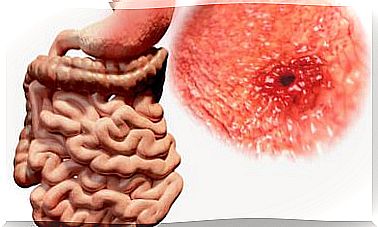
The liver is an organ that contains inside one tubes known under the name of bile ducts. The function of these structures is to drain a fluid from the liver called bile. The filtrate passes to the intestines and kidneys.
Bile is essential for proper digestion and carries waste substances from the liver to the intestine and kidneys to eliminate them.
A person with biliary atresia has these bile ducts blocked, so the bile cannot leave the liver. In this way, this organ is damaged, affecting many vital bodily functions.
On the other hand, it is worth mentioning that biliary atresia is the most common cause of liver transplantation in children living in the United States. It occurs once every 18,000 births and is more common in women than in men. Also, Asian, African American, and premature babies tend to get this disease more often compared to Caucasian babies.
Causes of biliary atresia
Today the causes responsible for the development of this disease are still not known. Some researchers believe that babies are born with the disease, so the disease could be triggered during pregnancy, when the liver is developing.
Other experts believe that the disease appears after birth, possibly due to exposure to toxic or infectious substances.
At first it is believed that biliary atresia is not associated with medications that the mother has taken, illnesses that she has had, or with anything that the mother has done during pregnancy.
Currently it is also unknown if there is a genetic relationship in the development of the disease, in addition, it is unlikely that the disease recurs more than once in a family.
What are the symptoms?
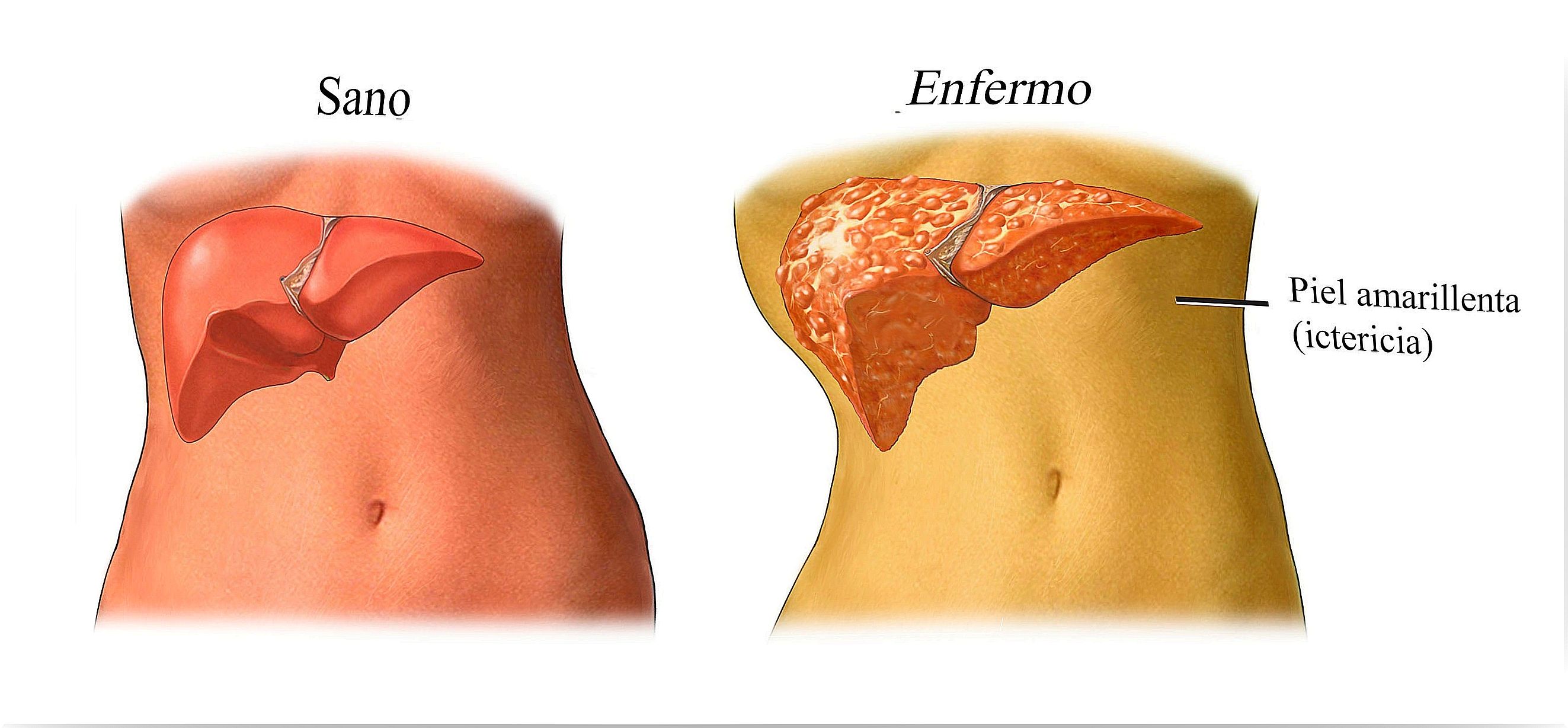
Newborns with this condition may appear normal at birth, however, jaundice (a yellowing of the skin and mucous membranes) develops by the second or third week of life.
The baby can gain weight normally during the first month. After that time, you will lose weight, become more irritable, and have worsening jaundice. Besides it, you can also develop other symptoms such as:
- Slow growth
- Pale or clay-colored stools
- Dark urine
- Little or no weight gain.
- Splenomegaly (enlarged spleen).
Treatment of biliary atresia
The therapeutic management of biliary atresia is very controversial, since 80-855 of those who suffer from the disease will end up undergoing a transplant.
In addition, as we have already mentioned, it is an irreversible disease and there are no medications that can unblock the bile ducts or promote the development of new bile ducts. Today, Kasai portoenterostomia is considered the first line of treatment.
However, as we mentioned, it is controversial, since many experts defend the advantages of this intervention as a first line compared to others who defend transplantation as a first option.
Kasai Portoenterestomy
This operation aims to connect the bile drainage from the liver directly into the intestinal tract. The Kasai portoenterestomy is most effective if it is done before the child is 3 months old.
In addition, it helps the child to grow and be in relatively good health for many years. However, it is important to bear in mind that cholestasis can occur, which is an accumulation of bile in the liver and that can lead to liver damage.
Liver transplant
As its name suggests, this surgery consists of transplanting a liver for a healthy one. This new organ can come from a deceased donor, part of a liver from a deceased donor, or part of a liver from a relative or other person whose tissue type is compatible with the patient’s tissue type.
After surgery, a child’s health usually improves rapidly, although he will need drugs to prevent the body from rejecting the new organ. This rejection is a normal protective mechanism of the body that tries to defend ourselves against viruses, tumors and other foreign substances.