Anthrax Treatment
Anthrax is a serious bacterial disease that primarily attacks the skin. In fact, cases in which it affects the oropharynx, the lower respiratory tract, the mediastinum, or the intestines are rare. The cause is the infectious agent called Bacillus anthracis, an immovable and encapsulated bacillus that is responsible for creating spores.
According to Vidal Gonzalo Rodríguez Lemoine, it was the French physicist Casimir Davaine who demonstrated in 1863 that the presence of bacillary forms found in the blood of animals with anthrax was an essential condition to produce death in inoculated animals.
In addition, this expert stated that they were bacteria and proposed the name Bacillus anthracis to designate them. However, Devaine’s ideas were not universally accepted, nor were his experiments conclusive.
Symptoms of the disease

In reality, the symptoms are not general, as it varies according to the way in which the infection was acquired. However, in most cases symptoms appear within the first 7 days. They are specifically defined below:
- Cutaneous route: more than 90% of anthrax infections occur when the bacteria penetrate the skin and form a wound or burn when the contaminated object is handled. At the beginning there is a lump that produces itching —similar to an insect bite—; After two days, it becomes a blister and, later, an ulcer.
- Inhaled form: the first symptoms are very similar to a common cold. However, within three days, respiratory problems and radiological signs of mediastinal widening and shock become severe. A large percentage of these cases end in death.
- Intestinal route: this form of contagion is the most difficult to identify. In some cases, it can be mistaken for an outbreak caused by food poisoning. It happens when a contaminated food is consumed ined and inflamed the intestinal tract. Its symptoms include nausea, vomiting, poor appetite, fever, abdominal pain, and severe diarrhea.
Diagnosis

The first thing that is taken into account when making the diagnosis is the existence of an epidemiological history. In other words, the doctor must specify whether the patient was exposed to the Bacillus anthracis germ or its spores.
Although this microorganism can attack anyone, in general it is more likely to be contracted by trades in which it has contact with animals, for example, livestock, farms or veterinarians. Fortunately, the incidence is low.
To determine that the patient is infected, a thorough clinical analysis is required and also tests to confirm it.
- Laboratory tests: blood, tissue samples, cerebrospinal fluid, or respiratory secretion.
- Antibody measurement or toxins in the blood before prescribing any antibiotics.
Anthrax treatment
If done properly and at the right time, anthrax treatment will make the difference between life and death.
Damage caused by anthrax must be emptied in order to heal. This process occurs in less than 15 days. One way to speed up healing if you have attacked the skin is to put warm, moist compresses on it. for the wound to heal.
If symptoms last longer than 2 weeks, treatment should be more rigorous so that there is no re drop.
It should be noted that throughout the entire process, hygiene is essential. Not only do you have to wash the affected area immediately and bathe, but you also have to disinfect clothing and seek medical assistance.
Frequently used antibiotics
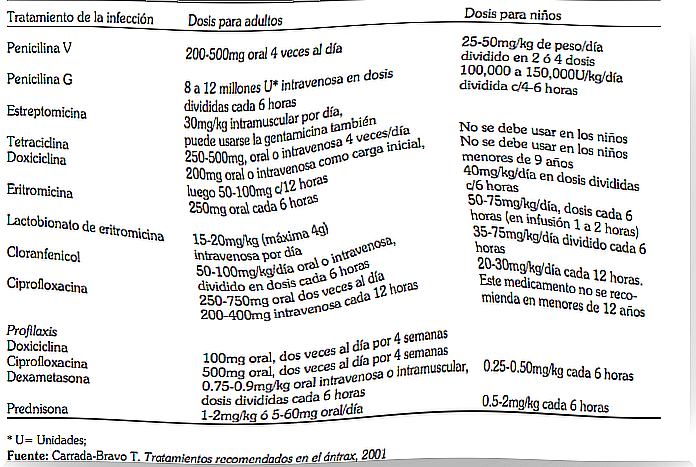
According to Dr. Teodoro Carrada Bravo, in cutaneous or complicated anthrax, the treatment of choice is oral penicillin ; in case of resistance, ciprofloxacin can be added.
On the other hand, in patients allergic to penicillin, chloramphenicol, erythromycin, tetracycline or ciprofloxacin can be used. It is prudent to note that ciprofloxacin and tetracyclines cannot be used in pregnant women or children; in vitro, anthrax strains are often resistant to cefuroxime.
Carrada also indicates, in reference to the treatment of anthrax, that in the most serious cases the following can be used:
- Penicillin.
- Doxycycline.
- Gentamicin.
- Ciprofloxacin.
- Erythromycin lactobionate.
For children, only high-dose penicillin, erythromycin lactobionate, and chloramphenicol 65-67 can be used.
Finally, it must be said that surgical excision of the eschar cannot be attempted due to the risk of post-surgical bacterial reactivation. Skin lesions should be covered with sterile gauze and, before disposing of contaminated materials, it is recommended to autoclave or incinerate them.